Home > ASME Articles > Study Participants Who Remained on Medication Treatment for OUD Post-Trial Had Better Outcomes at 36 Weeks
Addiction Science Made Easy
May 2021
Meg Brunner, MLIS
CTN Dissemination Librarian
http://ctndisseminationlibrary.org
Opioid use disorder (OUD) is a chronic, relapsing condition with serious consequences for individuals, communities, and public health. The FDA has approved 3 medications for the treatment of OUD (MOUD): methadone, buprenorphine, and naltrexone (typically extended-release injectable naltrexone). Despite their proven effectiveness, however, these medications are still underused, and most individuals with OUD are not receiving treatment.
Of those who do begin treatment with MOUD, the majority don’t remain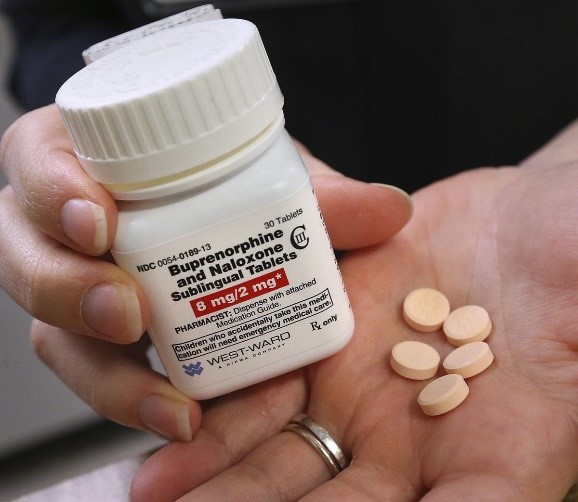 in treatment and are at high risk for relapse and overdose after discontinuing medication. Clinical trials have shown rates of under 50% for treatment retention, with most studies reporting on buprenorphine or methadone.
in treatment and are at high risk for relapse and overdose after discontinuing medication. Clinical trials have shown rates of under 50% for treatment retention, with most studies reporting on buprenorphine or methadone.
Naturalistic outcomes data – data obtained once participants have left a study’s structured setting and are back in their communities – are important to better understand OUD patients’ treatment trajectories and outcomes. The National Drug Abuse Treatment Clinical Trials Network (CTN) protocol CTN-0051, which compared extended-release naltrexone with buprenorphine-naloxone for opioid use disorder treatment, offered the opportunity to examine naturalistic MOUD use and opioid use outcomes in a 36-week follow-up of study participants (participants stopped receiving study medications at 24 weeks and were referred to community organizations to continue care).
Of the 428 participants who completed the 36-week visit, 225 (53%) were receiving MOUD and 203 (47%) were not. Compared to those off medication, participants on medication:
There was no difference in abstinence rates between those on or off MOUD. A greater proportion of participants on extended-release injectable naltrexone (53.4%) were abstinent from non-prescribed opioids compared to those on buprenorphine (23.3% of participants).
Conclusions: This look at naturalistic outcomes data showed that despite potential barriers to continuing treatment in their communities, about half of individuals were still on opioid use disorder treatment medications at follow-up, and those on medication generally had better outcomes. Future research is needed to explore ways to overcome barriers and keep people in treatment in community settings and to develop interventions tailored to improve treatment adherence and engagement.